你知道雙磷酸鹽類也有drug holiday之說嗎?
常見骨質疏鬆症用藥包括雙磷酸鹽類、RANKL mab、SERM、PTH衍生物…
其中,雙磷酸與denosumab有一個副作用叫做” 非典型股骨骨折”,啊我要預防骨折,吃一吃煞變成增加骨折? 這是哪招?
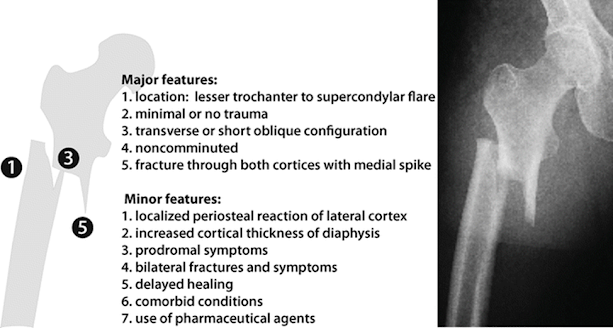
根據這篇N Engl J Med 2020; 383:743-753,非典型股骨骨折定義為發生在股骨diaphysis或是subtrochanteric位置的骨折。
統計發現亞洲人更容易出現非典型股骨骨折,風險因子包括>65歲、亞洲人、女性、長期類固醇治療、長期雙磷酸鹽類藥物。
雙磷酸鹽用越久越容易非典骨折,同理停越久越不容易非典骨折。然而非典骨折本身的發生率其實不太高,平均約1.74次/1萬人年;相比之下典型的髖關節骨折58.9次/1萬人年,差了33倍
因為雙磷酸鹽可以蓄積在骨頭中,有人建議雙磷酸鹽口服用5-10年、針劑用3-6年後,先停一陣子(drug holiday),可以維持防典型骨折效果,也可慢慢降低非典骨折與ONJ機率。Ther Adv Musculoskelet Dis. 2013 Jun; 5(3): 107–111.
l Fracture
Intervention Trial (FLEX)
研究高骨折風險女性(T<-2.5)吃了5年的alendronate,之後再吃五年藥VS吃五年安慰劑,發現吃藥組多3.8% 脊椎骨密度,脊椎骨折發生率與安慰劑組相比~2% vs 5% (relative risk 0.45 p=0.013 顯著有差)、非脊椎骨折15% vs 28%。所以高骨折風險者,建議持續吃藥。
l HORIZON
pivotal fracture trial
IV zoledronate 3年,再分IV 3年藥 vs IV 3年安慰劑,發現兩組骨密度差不多。但morphometric vertebral fractures(測脊椎長度判斷骨折與否)治療組vs安慰劑組=14 vs 30, OR 0.51, CI 0.26–0.95, p = 0.035,給藥組發生骨折次數稍微較少。所以若此人骨折險較高,繼續IV治療有好處
l 提到雖然有ONJ與非典骨折的議題,但其實發生率真的很低,所以不一定要為了他們而停藥 (然而沒有共識)
l 但大方向是,高骨折風險病人(T<-2~2.5),不建議drug holiday,或至少用6-10年以上再drug holiday。真的ha下去後也可以考慮給個非磷酸鹽類藥物如raloxifene
或teriparatide。
l 低骨折風險病人(T>-2.5 或 一直都沒有骨折)可考慮3-5年後開始drug holiday,但可Ha多久取決於藥物的骨頭親和性,與病人的典型骨折骨折風險,(也許亦可參考非典骨折風險),或者直到又骨折了,就趕快用回去。
骨頭親和性: zoledronate > alendronate > > risedronate
(親和性越差者,holiday越短,如risedronate 1年內重新評估是否用回藥物、alendronate 1-2年、zoledronate 2-3年)
病人的典型骨折骨折風險: >65歲、女性、T-socre、長期corticosteroid
非典骨折風險: >65歲、亞洲人、女性、長期類固醇治療、長期雙磷酸鹽類藥物
l 這個holiday玩意兒,only for雙磷酸鹽,denosumab, Forteo等藥都沒有這回事,沒副作用就該一直用下去,有副作用就換藥。
l Endocr Pract. 2020 May;26(Suppl 1):1-46. https://pubmed.ncbi.nlm.nih.gov/32427503/
根據2020美國臨床內分泌醫師協會指引: 雙磷酸鹽的drug holiday可以這麼做
Ref:
1. https://jtp.taiwan-pharma.org.tw/139/004.html
2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3707342/
3. https://www.nejm.org/doi/full/10.1056/NEJMoa1916525
l 骨折風險評估,使用fracture
risk assessment tool (FRAX®)
舉例:
1. Low risk of fracture: treatment
is not needed. If a bisphosphonate has been prescribed, it should be
discontinued and not restarted unless/until the patient meets treatment
guidelines.
Example: 54-yearold woman, menopause at age 51, lowest T-score –1.5, no risk
factors, bisphosphonate therapy for 3 years. Treatment was not indicated in the
first place and can be discontinued.
2. Mild risk of fracture: treat with bisphosphonate for 3–5 years, then
stop. The ‘drug holiday’ can be continued until there is significant loss of
BMD (i.e. more than the least significant change as determined by the testing
center) or the patient has a fracture, whichever comes first. Example: 68-year-old
woman, menopause at age 50, initial lowest T-score –2.3, parent with a hip
fracture, bisphosphonate treatment for 5 years, BMD stable over that time. Treatment
was indicated, but a drug holiday might be considered after 5 years of treatment.
3. Moderate risk of fracture: treat with bisphosphonate for 5–10 years,
offer a ‘drug holiday’ of 3–5 years or until there is significant loss of BMD
or the patient has a fracture, whichever comes first.
Example: 72-year-old woman, menopause at age 48, lowest initial T-score –2.8,
no risk factors, bisphosphonate therapy for 7 years, BMD
4. High risk of fracture (fractures,
corticosteroid therapy, very low BMD): treat with bisphosphonate for 10 years,
offer a ‘drug holiday’ of 1–2 years, until there is significant loss of BMD or
the patient has a fracture, whichever comes first. A non-bisphosphonate
treatment (e.g. raloxifene or teriparatide) may be offered during the ‘holiday’
from the bisphosphonate.
Example: 75-year-old woman, menopause at
age 45, lowest initial T-score –3.6, rheumatoid arthritis requiring ongoing
corticosteroid therapy for 12 years, two vertebral fractures by vertebral
fracture assessment (VFA), treatment with bisphosphonate therapy for 10 years.
Treatment was indicated and she remains at high risk of fracture after 10
years. If a holiday from the bisphosphonate is considered, interval treatment
with teriparatide or raloxifene would be prudent.







沒有留言:
張貼留言